What I love about RPA is it most often has the highest impact where there is a serious amount of IT failure, disorganization and overworked staff. Yes, that’s a lot of organizations to consider, and it’s one of the reasons why its hard to find this technology sexy – it’s built to fix the murky, dysfunctional stuff that has been squirreled away for decades, buried deep beneath failing ERP projects and conveniently ignored by senior executives who have few political points to score by acknowledging they should actually focus on fixing their broken underbellies.
This has been the failure of operations leaders for decades – simply focusing on layering more garbage over the top, when the real way to fix their inherent problems of dysfunction is to dig deep beneath their navels and address their broken process chains, and – heaven forbid – actually start to do something differently.
And there is no ground more fertile than the hallowed turf of the British National Health Service (NHS), the world’s sixth-largest employer with 1.7m staff, where decades of hollow political rhetoric, obscene wastage on ‘big-bang IT transformations” and big-ticket consultants on the gravy train, bravely held together by a woefully understaffed administration that end up spending on contract agencies just to keep the wheels turning. Let’s face facts: the UK National Health Service makes the basket-case that is Obama Care resemble a slick, well-oiled machine.
Enter RPA: a tool that is reducing GP referral processing time by 75%
But there is renewed hope – and this hope can quite easily become reality if you entertain the idea of using RPA to unify document submissions, scrape data from legacy desktops to speed up GP referral times. And the real value to be gained here is if the NHS can adopt a common enterprise-wide strategy to deploy a common RPA as-a-service toolset and methodology across its 207 individual trusts. It’s so simple, I describe in on the back of an envelope:
Even in these tough times for the institution, many of its leaders are looking optimistically at the opportunities new technologies that can be customized provide, which can solve business inefficiencies and don’t involve the massive complexities of entire system upheavals. One particular example provides insights into how one NHS trust is actively addressing some of these issues, both in terms of saving the NHS money directly, easing pressure on administrative staff and providing a better more consistent service for patients being referred to hospitals. All of these endeavors are in line with the broader objective of ensuring that the NHS meets some overriding objectives to digitize services.
The starting point for this work began at the East Suffolk and North Essex Foundation Trust (ESNEFT). The organization faced many of the same pressures discussed above and like all healthcare services within the UK, they were directed to enable all GP referrals to be processed via the Electronic Referral Service (eRS) by October 2018. However, the existing system for processing electronic referrals was based on manual processes and was slow—a common challenge.
Essentially, once the GP had made a referral to the Trust, the support staff have to find information such as scans, blood tests, and other results which need to be manually downloaded and appended to the file. In a process which may seem bizarre to many enterprises, this often meant admin staff were required to print off material and then scan it back into the same computer (using the same printer and scanner) to create a PDF file to navigate bottlenecks between unintegrated systems. The PDF document is then uploaded to the administration system. Approximately, this process took around 20 minutes for each referral and created, what the trust described as an avalanche of admin, distracting medical secretaries from their primary task of supporting patients and consultants.
ESNEFT had already started a pilot scheme looking to automate some accounts payable processes with the RPA provider Thoughtonomy, which was showing a great deal of promise. So, the Trust decided to use the system to automate the referral process across five clinical specialties, using “Virtual Workers” (BluePrism bots), which actively monitor incoming referrals from GP patient appointments in real-time, 24 hours a day. Once triggered, the Virtual Worker extracts the reason for referral, referral data, and supporting clinical information and merges the information into a single PDF document. This combined document is then uploaded into the Trust’s administrative systems. The RPA system uses virtual smart card technology for authentication providing the same level of data security assurance as the old manual process. Overall, the complete task now takes less than five minutes. The Virtual Workforce is able to update all systems, instantaneously and extract critical information, which it passes on to the lead consultant for review and grading.
One of the most important aspects of this technology is its ability to work within the current system, regardless of how chaotic and unstructured that may be. It is technology that adapts to the real world and the way people actually behave and work rather than expecting people to miraculously change current tropes and behaviours. This is perhaps the single most important reason RPA works: it provides whatever shaped peg is required, no matter the hole.
RPA negates the need to spend vast amounts on many complex technology integration projects
This first stage has significant cost savings—estimated to be $275,000 in the first year—without removing staff. Crucially, the $275K saving achieved is made up of agency staff and sundry costs such as printing. ESNEFT believe that 500 hours of time was saved thanks to the solution. Plus it increased the job satisfaction of the admin staff, who could concentrate on more important aspects of their role.
For us, although the top line cost saving number is important, it’s the fact that a technology solution proof of concept has been deployed successfully (and relatively painlessly) within the NHS. To deliver the outcome required, there was no need to drive an enormous transformation project to align and integrate systems. Which, given the lack of appetite for big bang projects in the NHS is an achievement in itself. Simply put, the way the technology is used can be fitted into the existing chaos—it’s technology for the real world. It can provide a bottom-up solution to productivity improvements, which is a project that replaces part of existing work flows and automates manual and repetitive tasks. It accomplishes these things with the double whammy of removing tasks which is disliked, genuinely improving outcomes to patients, whilst helping to drive efficiency.
Bottom line: The NHS is not alone in facing an unforgivingly complex estate, but with technologies that fit into the chaos of the modern organization, this is only the start
If we look more broadly at the impact RPA technology could have on the NHS, we can use a simple calculation to estimate the ramifications this technology can have. We know that savings of $275K have been made on 2,000 GP referrals per week. But the figure for NHS England as a whole, puts GP referrals at 3.5m from April 2018 to June 2018. So, if this were scaled up, we could see savings across NHS England purely for GP referrals at a staggering $38m, this included all hospital referrals the figure rises to almost $63m, or around $1.3m per week. To put this in context, this would equate to almost 850 nurses for the GP referrals or almost 1,400 for all referrals in England (using the average cost of $45,000 per annum for a mid-tier nurse, source: Nuffield trust).
This is the tip of the iceberg, considering that more than 520M working hours are currently spent on admin and approximately $3.3 billion is spent on agency staff across the NHS as a whole during 2016. There is a great deal of savings to be had. Even if only a quarter of the agency spend is non-medical, that could be $820M per year that could be freed up with only positive impacts on patient outcomes.
Posted in : Healthcare and Outsourcing, Robotic Process Automation

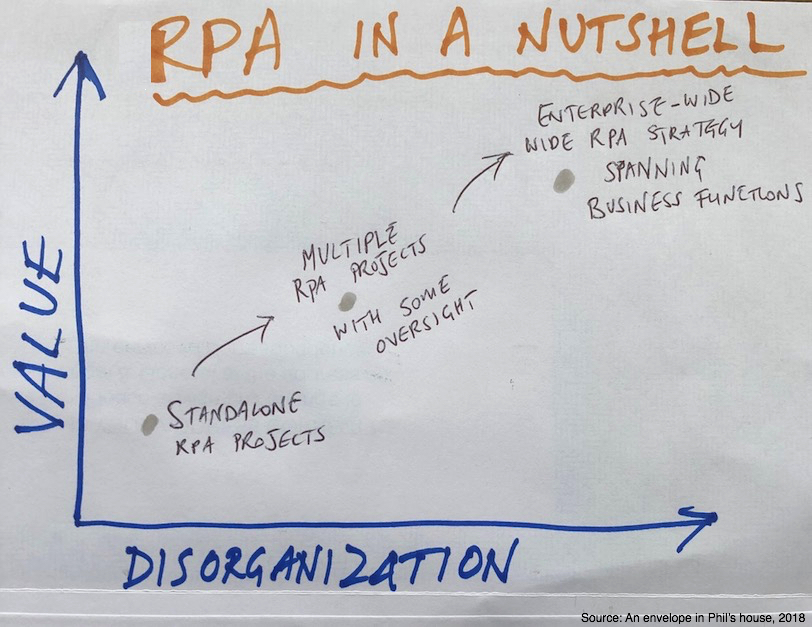




Love the graphic. Simple. Direct. Correct.
Combination of cleaning processes then automating – win win. More work and a slightly different project than clients expect at the beginning but the ROI (and I’m not only referring to cost saving) can be phenomenal.
Someone needs to stuff this research down Matt Hancock’s throat. Great post.
Thanks for this great example of RPA in action including cost savings, which tool, and the process details. It’s helpful to see specific examples written about to see the possibilities of RPA.